
Derangements in any factors can affect clotting ability. The blood clotting cascade is an integral system requiring intrinsic and extrinsic factors. Review laboratory results for coagulation status as appropriate: platelet count, prothrombin time/international normalized ratio (PT/INR), activated partial thromboplastin time (aPTT), fibrinogen, bleeding time, fibrin degradation products, vitamin K, activated coagulation time (ACT).
many drugs used to treat cancer suppress bone marrow function and therefore the production of platelets. Heparin, a parenteral anticoagulant, inhibits the action of thrombin and prevents formation of a fibrin clot.

Warfarin, an oral anticoagulant, inhibits the synthesis of vitamin K in the liver, thus reducing levels of several subsequent clotting factors. Salicylates and other NSAIDs inhibit cyclooxygenase 1 (COX)-1, an enzyme that promotes platelet aggregation.
Orthostasis (a drip of 20 mm Hg in systolic BP or 10 mm Hg in diastolic BP when changing from supine to sitting position) indicates reduced circulating fluids.Įvaluate the patient’s use of any medications that can affect hemostasis (e.g, anticoagulants, salicylates, NSAIDs, or cancer chemotherapy).ĭrugs that interfere with clotting mechanisms or platelet activity increase risk for bleeding. Hypotension and tachycardia are initial compensatory mechanisms usually noted with bleeding. Look for signs of orthostatic hypotension. Monitor patient’s vital signs, especially BP and HR. Herbal remedies may be connected to bleeding problems through a direct effect on clotting factors or interactions with anticoagulants.ĭetermine the patient’s health history for signs that can be associated with a risk for bleeding such as liver disease, inflammatory bowel disease, or peptic ulcer disease.Įarly identification of possible risks for bleeding provides a foundation for implementing appropriate preventive measures. Bleeding is the primary complication of anticoagulant therapy and is a risk of all anticoagulants even when maintained within the usual therapeutic ranges. These drugs include anticoagulants, nonsteroidal anti-inflammatory drugs ( NSAIDs), and cancer chemotherapy agents. Drugs may also be the reason why a patient’s bone marrow function is suppressed which increases the patient’s risk for bleeding. Examples of these conditions include traumatic injury, major organ surgery, and the many inflammatories and ulcerative disorders of the gastrointestinal system like inflammatory bowel disease and peptic ulcer disease. Risk for bleeding may arise in any condition that disturbs the “close circuit” integrity of the circulatory system.
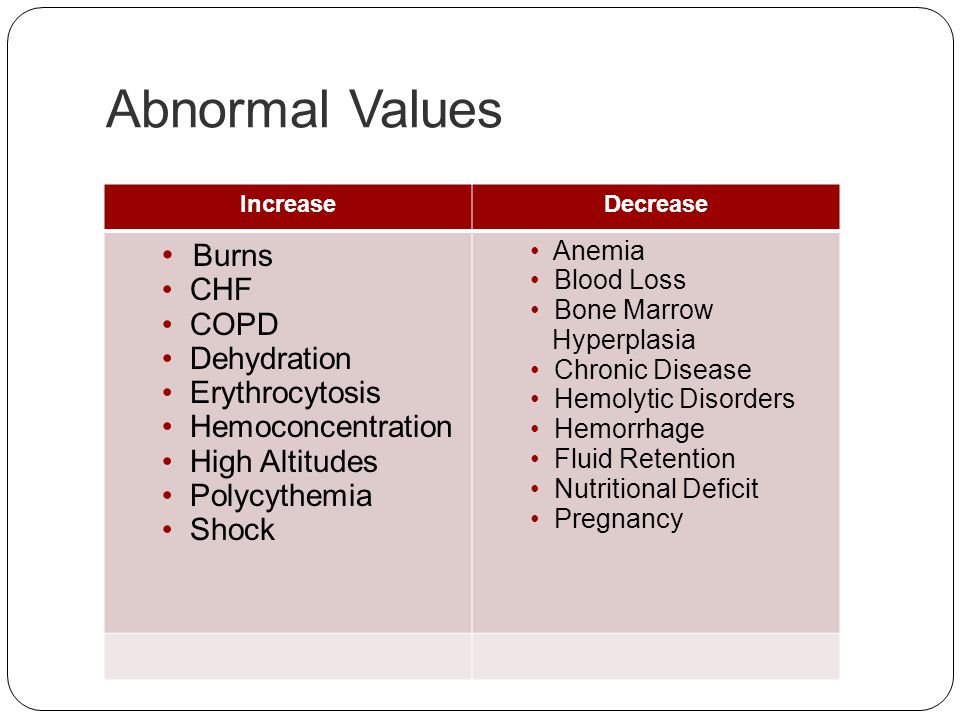
Reduction in the synthesis of clotting factors is due to liver impairment. Increased destruction of platelets is linked to immune thrombocytopenic purpura (ITP). A reduction in production of platelets from the bone marrow is linked to cancers of the blood and blood-forming organs. Risk for bleeding happens with disorders that reduce the quality or quantity of circulating platelets (thrombocytopenia). Certain diseases like hemophilia interfere with genetic expression of normal clotting factors. When disease or the outcome of disease treatments confuse the standard mechanisms that maintain hemostasis, a patient may be at risk for bleeding. Therapeutic Communication Techniques Quiz.


 0 kommentar(er)
0 kommentar(er)
